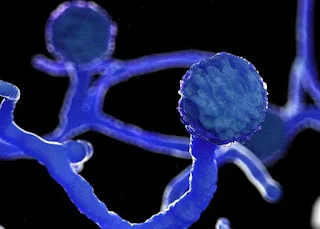
How Can Black Fungus (Mucormycosis) Spread?
Black fungus, medically known as mucormycosis, is a serious but rare fungal infection. Although it surged during the COVID‑19 pandemic, most people are at low risk. Understanding its pathways helps stop spread and protect vulnerable individuals.
Transmission from the Environment
Mucorales fungi thrive in soil, compost, decaying organic matter and even mouldy masks or linens. You can't catch it from another person—only from spores in the environment :contentReference[oaicite:3]{index=3}.
- Inhalation: Breathing in airborne spores can infect the sinuses or lungs :contentReference[oaicite:4]{index=4}.
- Ingestion: Eating contaminated food may lead to gastrointestinal infection.
- Inoculation: Spores entering via cuts or wounds can cause cutaneous infection—even in healthy skin :contentReference[oaicite:5]{index=5}.
Outbreaks in Healthcare Settings
Hospitals occasionally see mucormycosis outbreaks due to contaminated equipment or linens:
- Non‑sterile bandages or tongue depressors
- Poorly washed linens or negative‑pressure rooms
- Dust during hospital renovations or leaks :contentReference[oaicite:6]{index=6}
These healthcare-associated outbreaks are rare but can be serious :contentReference[oaicite:7]{index=7}.
Spread Within the Body
Once spores enter, the fungus can spread rapidly:
- Sinus or pulmonary entry: Spores lodge in the sinuses or lungs and grow.
- Angioinvasion: They invade blood vessels, causing clots and tissue death :contentReference[oaicite:8]{index=8}.
- Dissemination: The infection can spread via the bloodstream to the brain, skin or other organs :contentReference[oaicite:9]{index=9}.
Not Contagious Between Humans or Animals
Mucormycosis cannot be passed from person to person or through animals. Transmission requires direct contact with spores in the air, soil, food, or contaminated items :contentReference[oaicite:10]{index=10}.
Real-Life Observations
During India’s COVID‑19 surge, over 40,000 cases were reported—mainly due to inhaled spores combined with weakened immune systems, steroid use, and high blood sugar :contentReference[oaicite:11]{index=11}.
When to Suspect Transmission
- New sinus/lung symptoms after hospital stays or exposure to contaminated materials
- Black lesions on the nose, mouth, or skin
- Unusual infections following trauma or natural disasters
Prevention Strategies
- Avoid dusty environments and use masks when gardening
- Discard or wash reusable masks, gowns, and linens properly :contentReference[oaicite:12]{index=12}
- Manage diabetes and use steroids only as prescribed during COVID‑19 :contentReference[oaicite:13]{index=13}
- Ensure hospitals follow infection-control protocols during construction or linen handling :contentReference[oaicite:14]{index=14}
FAQs
- Can I catch black fungus from another person? No—it's not contagious.
- Can healthy people get it? Rarely—mostly after skin trauma or heavy spore exposure :contentReference[oaicite:15]{index=15}.
- Is hospital-acquired mucormycosis real? Yes, but rare—linked to contaminated materials or dust :contentReference[oaicite:16]{index=16}.
Internal References
Final Thoughts
Black fungus spreads only from environmental spores or contaminated items—not person-to-person. Awareness of its routes, early symptoms, and strict hygiene—especially in healthcare settings—can help keep you safe.